Comprehensive Cleft Lip & Palate Management Protocol
- Get link
- X
- Other Apps
if you are intersted in this article please follow for more readings
Outline:
1. Introduction
2. Treatment goals
3. Prenatal period
4. Neonatal period
5. 6 months to 2 years
6. 2 to 7 years old
7. Mixed dentition
8. Permanent dentition
9. References
1- Introduction
Cleft lip and palate (CLP) is the most frequent congenital facial abnormality. Its incidence varies according to studied populations but is usually between 1 and 1.82 % for each 1000 births.1
Children with cleft lip and palate may experience a multitude of physical and developmental challenges. There also may be psychosocial and emotional concerns for the patients and their families.2
As such, management of patient with
cleft lip and palate should go through a multidisciplinary team who will
provide the optimal treatment.3
The managing team should provide
comprehensive diagnosis, planning, and treatment. The cleft team usually
includes 4 :
1-Orthodontist
2-Maxillofacial surgeon
3-Plastic surgeon
4-Prosthodontist
5-Speech therapist
6-Audiologist (ENT specialist)
7- Psychologist
7-Pediatrician.
1- Treatment goals
Treatment goals should include5 :
-
The
correction of birth defects (lip, palate, and nose)
-
Achieving
normal speech,
-
Hearing
-
Language
-
Occlusion
-
Maintaining
good dental health.
-
Optimize
the psychosocial outcomes
-
Developmental
outcomes.
1-
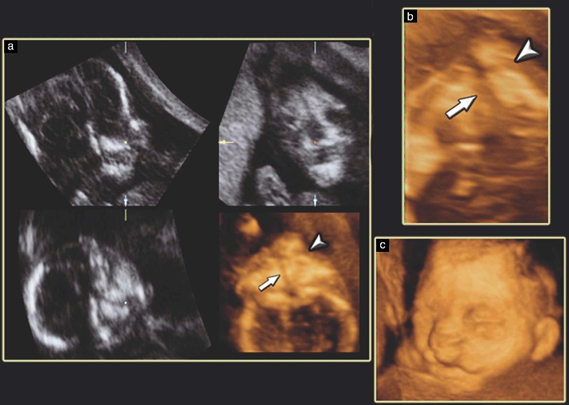
Prenatal period
Ultrasound examination can detect clefts of the lip and alveolus
unlike cleft palate, which is difficult to diagnose through routine screening.3
2 dimension
ultrasound in conjunction with 3D ultrasound improves the detection rate for
fetal cleft lip and palate, compared with 2Dultrasound alone.6
Prenatal diagnosis enables appropriate and timely counseling of the parents by the cleft team and helps instill a sense of preparedness for the family which highly improves the quality of treatment received by the child enabling a near-to-normal quality and standard of life.
1-
Neonatal period: 2 weeks to 6 months
The most immediate problem caused by orofacial
clefting is likely to be difficulty with feeding. The anatomical
characteristics of cleft lip and palate greatly hinder infants’ ability to
feed.
Poor intraoral suction may produce choking, nasal discharge and excessive time required to take nourishment.
Early consultation to the infant-feeding specialist or nurses associated with cleft teams can help in solving this problem. Another solution is also available, the use of the acrylic plates (palatal plate) that are designed to help with the feeding or to move the displaced cleft segments towards a more normal relationship in order to aid subsequent surgical apposition. This is known as pre-surgical orthopedics 8
Presurgical orthopedics and nasoalveolar molding have become part
of the treatment protocol in many cleft centers to improve the treatment
outcome. 8
a- Feeding:
Squeezable bottles more easily than rigid feeding bottles for babies born with clefts of the lip and/or palate, however, however, it doesn’t differ in growth outcomes between the bottle types. No need for the use of different types of maternal advice and/or support for these babies. 9
a- Nasoalveolar
Molding:
It is done by the
orthodontist serving on the cleft palate and cranio- facial team. With the use
of an intraoral molding appliance and extra-oral taping, the alveolar ridges
are approximated by 1 to 2 mm to each other.
Nasal stents can be added for lengthening of the columella in
bilateral cleft patients.2 Nasoalveolar molding appliance therapy offer:
-
Positive surgical,
-
Aesthetical,
-
Functional
and
-
Socio-economical
effects on unilateral clefts of the lip and/or palate treatment when performed
prior to primary repair surgeries.10
It can reduce the cleft gap, which, while preventing the arch
collapse, leads to improved, stable, and symmetric arch form at 6 years of age.
Significant reduction in cleft gap was also noted in the long term in control patients in whom presurgical nasoalveolar molding was not performed, but at the cost of anterior arch collapse leading to dental crossbite.11
a- Lip
repair:
Timing of Lip repair is when the infant is about 3 months of age. This timing has its roots in the “rule of 10s” advocated by Wilhelmsen and Musgrave (1966).8
The rule of 10s states that an infant should be :
-
A
least 10 weeks of age,
-
Weigh at least 10 pounds,
- Hemoglobin count of at least 10 grams prior to surgery.
The surgeon
experience and patient preferences are the main factors affecting the selection
of the technique for unilateral cleft repair. There is a rare randomized
controlled trials and prospective studies on whether open or closed rhinoplasty
during primary cleft lip repair gives better long-term outcomes.13 no significant different between Tennison-Randall (triangular)
technique or the Millard rotation-advancement technique in cleft lip repair.14
1-
From 6 month 2years old:
a- Primary
Alveolar Bone Grafting and Gingivoperiosteoplasty:
Many surgeons adopt the “early cleft repair” concept in which
attempts to achieve continuity in the alveolar bone are done during the first 2
years of patient’s life.
The primary
bone grafted patient demonstrated less vertical descent-of the anterior maxilla
compared to the gingivoperiosteoplasty and non-grafted patient.15
Very weak evidence indicated that Gingivoperiosteoplasty might not be assist in alveolar bone reconstruction for cleft lip and palate patient. Gingivoperiosteoplasty surgery could inhibit the growth of maxilla in cleft lip and palate patient.16
a- Palate
repair:
Hard and soft palate
repair is performed at the age range of 9–18 months.3
The early repair of the soft palate, when done with the lip repair,
and palate repair by two surgeries don’t affect the maxillary vertical and
sagittal dimensions and also don’t affect the mandibular morphology and spatial
positioning.
But, it has been suggested that total palate repair in a single
surgical time contributes poorly to the final maxillary retropositioning.17
1-
2 to 7 years old :
a-
Correction of speech defect:
Incompetency of
velopharyngeal and palatal mobility of the repaired cleft palate may result in
adaptations by the child which will lead hyper-nasality of speech and will lead
also to glottal stops.
To reduce the nasal air escape, a surgical pharyngeal flap is
needed in which the soft palate is connected permanently to the superior
anterior pharyngeal wall.2
Assessment of speech must continue through childhood along with cleft team to detect any developing problems that may arise with growth.3
a-
Lip revision surgery:
Lip revision and closure
of any residual palatal fistula before schooling might be considered to support
speech development.3
1-
Mixed dentition: 7 to 12 years:
At this stage the main goals of the treatment were to correct the
anterior and posterior crossbites, perform a bilateral secondary bone graft,
and perform dental alignment and leveling to achieve adequate intercuspation. In
addition to the occlusal alterations, balancing of the patient’s profile was
also desired.2
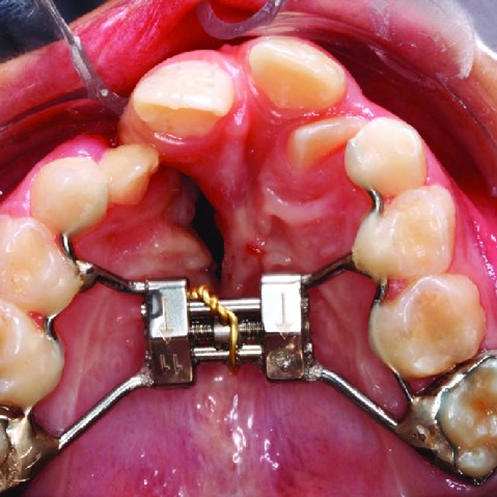
a- Maxillary
expansion:
No significant
different between rapid maxillary expansion and slow maxillary expansion in
sagittal and vertical expansion of maxilla in cleft lip and palate patient.18
It was found that hyrax
expander has better results in anterior and posterior maxillary expansion than
fan-type, and inverted mini-hyrax supported on the first premolars.
The inverted mini-hyrax best result in restricted posterior
expansion, optimizing anterior expansion without causing as much buccal tipping
of the supporting teeth as did the fan-type.19
a- Face
mask:
It was found that
rapid maxillary expansion and the Delaire facemask showed greatest
effectiveness in the lower midface soft tissue forward displacement and forward
rotation in the cleft lip and palate patients with class III cleft lip and
palate patients.20
The use of facemask with miniplate in growing unilateral cleft lip
and palate shows a more favorable change in maxillary advancement than the
bilateral cleft lip and palate patient.21
It is better to perform
maxillary protraction using a facemask with a miniplate anchorage than a
facemask with a tooth-borne anchorage and after alveolar bone graft rather than
before alveolar bone graft, regardless of cleft type.22
a- Secondary
bone grafting:
The best time for
alveolar bone graft to give the best results is located between 8 and 12 years,
before or just after the eruption of permanent canines adjacent to the cleft.
However, this timing could be modified by the multidisciplinary
team according priorities, particularly aesthetic, defined for each child.23
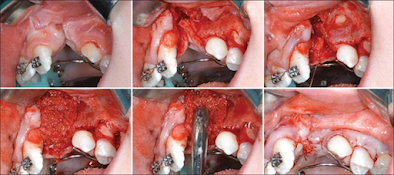
Tissue engineered bone substitutes give the same effect as
autogenous bone inreduction cleft volume, which creates the viable option of
eliminating the need for a second surgical site with its associated
postoperative morbidity.24
1-
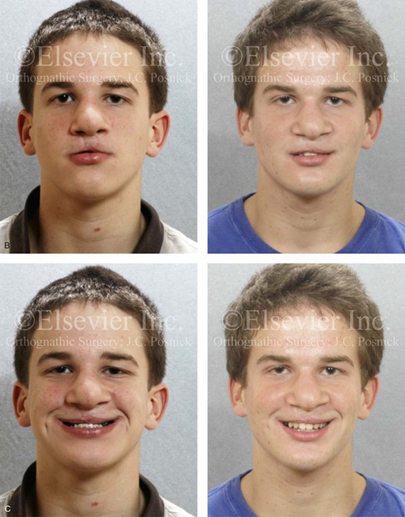
Permanent dentition: 12 years to adulthood:
As growth has been stopped and no longer moving of skeletal
discrepancies, surgical corrections of the skeletal and nasolabial soft tissue
revisions are planned.2
a- Comprehensive
orthodontic treatment:
A comprehensive treatment should be achieved, with same goals as a
non-clefting patient maintenance of the integrity of the dentition and
supporting structures especially for teeth adjacent to the cleft side,
correction of impacted and transposed teeth, and management of congenitally
missing teeth.2
It was found that
orthodontic space closure and prosthetic replacement gives similar result in
term of aesthetics. but in term of masticatory function orthodontic space
closure is much better than prosthetic replacement.25
a- Orthognathic
surgery:
Maxillary advancement
with distraction osteogenesis has good stability in cleft lip and palate patients with moderate and severe maxillary
deficiency.26 Maxillary advancement with distraction osteogenesis has no
advantage over congenital orthognathic for the purpose of preventing
velopharyngeal incompetence and speech disturbance in moderate maxillary
advancement in patient with cleft lip and palate.27
It was found that the amount of required maxillary advancement,
vector control of the palatal plane, and vertical position of the upper incisor
would be important factors when planning a surgical treatment whether by
maxillary advancement surgery with lefort I osteotomy or maxillary distraction
osteogenesis for cleft lip and palate patient.28
a- Surgical
revision:
Pharyngeal flap is
better than sphincter pharyngoplasty for velopharyngeal insufficiency resolution,
with no significant increase in complication rates.29
9-
References:
1. Rocha, R., Ritter, D. E., Locks,
A., de Paula, L. K., & Santana, R. M. (2012). Ideal treatment protocol
for cleft lip and palate patient from mixed to permanent dentition. American
Journal of Orthodontics and Dentofacial Orthopedics, 141(4),
S140–S148. doi:10.1016/j.ajodo.2011.03.024
2. Vig KWL, Mercado AM. Overview of orthodontic care for
children with cleft lip and palate, 1915-2015. Am. J. Orthod. Dentofac. Orthop.
2015;148(4):543–56. Available at:
http://dx.doi.org/10.1016/j.ajodo.2015.07.021.
3. Zreaqat M, Hassan R, Hanoun A. Cleft Lip and Palate
Management from Birth to Adulthood : An World ’ s largest Science , Technology
& Medicine Open Access book publisher. 2017;(September).
4. Schnitt DE, Agir H, David DJ. From Birth to Maturity : A
Group of Patients Who Have Completed Their Protocol Management . Part I .
Unilateral Cleft Lip and Palate. 2003:805–17.
5. Searle A, Neville P, Waylen A. Psychological growth and
well-being in individuals born with cleft: An application of self-determination
theory. Psychol. Health 2017;32(4):459–82. Available at:
https://doi.org/10.1080/08870446.2016.1275630.
6. Chmait R, Pretorius D, Jones M, et al. Prenatal evaluation
of facial clefts with two-dimensional and adjunctive three-dimensional
ultrasonography : A prospective trial. 2002:946–9.
7. Sreejith VP, Arun V, Devarajan AP, Gopinath A, Sunil M.
Psychological Effect of Prenatal Diagnosis of Cleft Lip and Palate: A
Systematic Review. Contemp. Clin. Dent. 2018;9(2):304–8. Available at:
https://pubmed.ncbi.nlm.nih.gov/29875578.
8. David J. Zajac LDV. evaluation and mangement of cleft lip
and palate. pluralpublishing; 2017.
9. Bessell A, Hooper L, Wc S, Reilly S, Reid J, Am G. Feeding
interventions for growth and development in infants with cleft lip , cleft
palate or cleft lip and palate ( Review ). 2011;(2).
10. Maillard S, Retrouvey J, Ahmed MK, Taub PJ. Correlation
between Nasoalveolar Molding and Surgical , Aesthetic , Functional and
Socioeconomic Outcomes Following Primary Repair Surgery : a Systematic Review.
8(3):1–15.
11. Shetty V, Agrawal RK, Long-term HFS. Long-term effect of
presurgical nasoalveolar molding on growth of maxillary arch in unilateral
cleft lip and palate : randomized controlled trial. Int. J. Oral Maxillofac.
Surg. 2017;46(8):977–87. Available at:
http://dx.doi.org/10.1016/j.ijom.2017.03.006.
12. Chow I, Purnell CA, Hanwright PJ, Gosain AK. Evaluating
the Rule of 10s in Cleft Lip Repair : 2016:670–9.
13. Jayarajan R, Natarajan A, Nagamuttu R. Outcomes of Closed
Versus Open Technique of Rhinoplasty During Primary Repair of Unilateral Cleft
Lip : A Systematic Review. 2018.
14. Adetayo AM, James O, Adeyemo WL, Ogunlewe MO, Butali A.
Unilateral cleft lip repair : a comparison of treatment outcome with two
surgical techniques using quantitative ( anthropometry ) assessment. 2018:3–11.
15. Grisius TM, Spolyar J, Jackson IT, Bello-Rojas G, Dajani
K. Assessment of Cleft Lip and Palate Patients Treated With Presurgical
Orthopedic Correction and Either Primary Bone Grafts, Gingivoperiosteoplasty,
or Without Alveolar Grafting Procedures. J. Craniofac. Surg. 2006;17(3).
Available at: https://journals.lww.com/jcraniofacialsurgery/Fulltext/2006/05000/Assessment_of_Cleft_Lip_and_Palate_Patients.13.aspx.
16. El-ashmawi NA, Ed M, Elkordy SA, et al. Effectiveness of
Gingivoperiosteoplasty on Alveolar Bone Reconstruction and Facial Growth in
Patients With Cleft Lip and Palate : A Systematic Review and Meta-Analysis.
2019;56(4):438–53.
17. Gabriel O, Calvano F. Craniofacial Morphology in Children
with Complete Unilateral Cleft Lip and Palate : A Comparison of Two Surgical
Protocols.
18. Arthur C, Greg L. Cephalometric evaluation of rapid and
slow maxillary expansion in patients with BCLP : Secondary data analysis from a
randomized clinical trial. 00(00):1–7.
19. Belo Horizonte, Minas Gerais, Brazil, and Cleveland O,
Introduction: Dentoskeletal effects of 3 maxillary expanders in patients with
clefts: A cone-beam computed tomography study. Am J Orthod Dentofac. Orthop
2014:73–81.
20. Hoefert CS, Bacher M, Herberts T, Krimmel M, Reinert S,
Göz G. 3 D Soft Tissue Changes in Facial Morphology in Patients with Cleft Lip
and Palate and Class III Mal occlusion under Therapy with Rapid Maxillary
Expansion and Delaire Facemask morphologie von Patienten mit LKG-Spalten und
Klasse-III-Anomalien unter Therapie mit Gaumen- nahterweiterung und
Delaire-Maske. 2010;(2):136–51.
21. Ahn H, Kim K, Yang I, Choi J, Baek S. Comparison of the
effects of maxillary protraction using facemask and miniplate anchorage between
unilateral and bilateral cleft lip and palate patients. 2012;82(5).
22. Yang I, Chang Y, Ph D, Kim T, Ph D. Effects of Cleft Type
, Facemask Anchorage Method , and Alveolar Bone Graft on Maxillary
Protraction : A Three-Dimensional Finite Element Analysis. 2008.
23. Elhaddaoui R, Bahije L, Zaoui F, Rerhrhaye W. Calendrier
de la greffe osseuse et séquences d ’ éruption canine dans les cas de fentes
labio-alvéolo-palatines : revue systématique. 2017:193–8.
24. Kamal M, Ziyab AH, Bartella A, Mitchell D, Al-asfour A,
Hölzle F. Volumetric comparison of autogenous bone and tissue-engineered bone
replacement materials in alveolar cleft repair : a systematic review and
meta-analysis. Br. J. Oral Maxillofac. Surg. 2018;(2017). Available at:
https://doi.org/10.1016/j.bjoms.2018.05.007.
25. Oosterkamp BCM, Dijkstra PU, Ph D, et al. Orthodontic
Space Closure Versus Prosthetic Replacement of Missing Upper Lateral Incisors
in Patients With Bilateral Cleft Lip and Palate. 2005.
26. Saltaji H, Major MP, Altalibi M, Youssef M, Flores-mir C.
Long-term skeletal stability after maxillary advancement with distraction
osteogenesis in cleft lip and palate patients A systematic review. 2012;82(6).
27. Chua HDP, Whitehill TL, Samman N, Maxillary LKC.
Maxillary distraction versus orthognathic surgery in cleft lip and palate
patients : effects on speech and velopharyngeal function. Int. J. Oral
Maxillofac. Surg. 2010;39(7):633–40. Available at:
http://dx.doi.org/10.1016/j.ijom.2010.03.011.
28. Baek S, Lee J, Lee J, Kim M, Kim J. Comparison of
Treatment Outcome and Stability Between Distraction Osteogenesis and LeFort I
Osteotomy in Cleft Patients With Maxillary Hypoplasia. :1–7.
29. Collins J, Cheung K, Farrokhyar F, Strumas N. Pharyngeal
flap versus sphincter pharyngoplasty for the treatment of velopharyngeal
insufficiency : Br. J. Plast. Surg. 2012;65(7):864–8. Available at:
http://dx.doi.org/10.1016/j.bjps.2012.01.020.
- Get link
- X
- Other Apps




















Comments
Post a Comment